Transcatheter aortic valve replacement (TAVR) procedures performed using transcaval or transaxillary access are associated with more complications than transfemoral TAVR, according to a new study published in JACC: Cardiovascular Interventions.[1] However, the authors noted, when nonfemoral access is required, transcaval TAVR “may offer an attractive option.” These alternative TAVR access routes are used when the preferred femoral access route is not usable because of anatomical issues, such has heavy calcium burden.
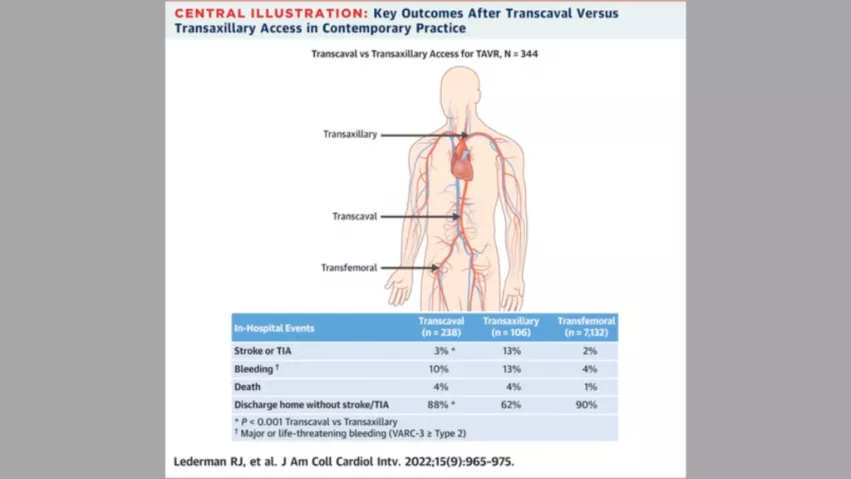
The group focused on data from eight different U.S. facilities. All procedures were performed from 2017 to 2020 and included in the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Overall, transcaval access was used in 238 procedures and transaxillary access was used in 106 procedures. During the same time period at the same facilities, more than 7,000 TAVR procedures were performed using transfemoral access.
“The key challenge to the current report is determining whether the comparisons between transcaval and transaxillary access are valid,” wrote lead author Robert J. Lederman, MD, a specialist with the division of intramural research at the National Heart, Lung, and Blood Institute, and colleagues. “First, are the patients equally sick and equally predisposed to complications? Although the patients were not randomly allocated to the access route, we used propensity score weighting to correct for between-group preprocedure imbalances.”
Overall, the authors reported, the stroke/transient ischemic attack (TIA) rates were 3% for transcaval TAVR and 13% for transaxillary TAVR. The rate of major and life-threatening bleeding events was also lower for transcaval TAVR than transaxillary TAVR (10% vs. 13%), but both treatment options had a mortality rate of 4%.
Transfemoral TAVR, meanwhile, had a stroke/TIA rate of 2%, major and life-threatening bleeding event rate of 4% and mortality rate of 1%.
Finally, the percentage of patients who were able to go straight home after discharge without a stroke or TIA was 88% after transcaval TAVR, 62% after transaxillary TAVR and 90% after transfemoral TAVR.
“In this report, transcaval access conferred a transfemoral-like low risk of stroke,” the authors wrote. “The reduced stroke risk persisted after adjustment for differences in baseline characteristics that might have influenced nonrandom treatment allocation. The proposed mechanism of stroke after transaxillary access is sheath instrumentation of atherosclerotic head and neck vessels. By contrast, transfemoral and transcaval procedures traverse the aorta without instrumenting the head and neck vessels. We infer, provocatively, that transcaval TAVR may prove the percutaneous nonfemoral access of choice; this requires more real-world experience in centers in and outside the United States.”
Related TAVR Content:
Henry Ford cardiologist leads first transcaval valve replacement in Europe
Transcarotid Access: The Future of Non-femoral TAVR?
Transaxillary TAVR emerges as top alternative to femoral access
Henry Ford Hospital pioneers new cardiac approach
TAVR outcomes unaffected when women require a smaller valve prosthesis
The latest data on mitral valve infective endocarditis after TAVR
VIDEO: TAVR durability outperforms surgical valves
How the continued rise of TAVR has impacted SAVR outcomes
Reference: