Quantitative flow ratio (QFR) allows for the functional assessment of stenosis on par with fractional flow reserve (FFR) but doesn’t require a guidewire, an international group of researchers reported in the Journal of the American Heart Association.
FFR has recently become recognized as the gold standard of physiological assessment of intermediate coronary stenosis, wrote lead author Jelmer Westra and colleagues. Armed with this knowledge, clinicians can make better decisions about whether to perform percutaneous coronary intervention (PCI) or not.
But uptake of FFR remains poor internationally, the authors noted, leading to interest in ways to approximate FFR using existing techniques such as coronary CT angiography and conventional coronary angiography.
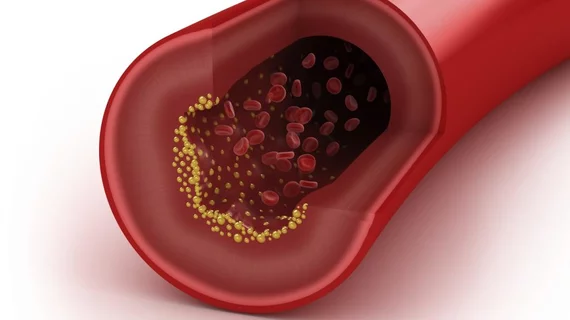
QFR is a computation of FFR based on a 3D reconstruction of the stenotic vessel rendered from two intra-procedure angiographic projections. In this analysis of 317 vessels from 272 patients with stable angina, QFR demonstrated better agreement with FFR than two-dimensional angiography for identifying significant vessel obstruction. Significant obstructions were defined as below 0.80 for FFR and QFR and above 50 percent diameter stenosis upon angiography.
Using FFR as a reference, the sensitivity and specificity of QFR for detecting stenosis was 86.5 percent and 86.9 percent, respectively. The corresponding values for angiography were 44.2 percent and 76.5 percent. Also, the area under the receiver curve was 0.92 for QFR versus 0.64 for angiography.
“We showed that QFR is superior to standard quantitative coronary angiography in evaluating coronary artery stenosis,” wrote Westra, with Aarhus University Hospital in Denmark, and colleagues. “QFR may extend the access to physiology‐based guidance when access to pressure wires is limited by financial restrictions or inexpedient reimbursement systems.”
QFR was not only feasible in a clinical setting but faster to calculate than FFR, which typically relies on computational fluid dynamics.
“Inherited limitations of these methods may exist related to generating theoretical boundary conditions to create a ‘one‐size‐fits‐all,’ and to long computation time for blood flow simulations,” the authors wrote. “To our knowledge, the FAVOR II studies using QFR present the first data supporting that real‐time computation of FFR is feasible, fast, and accurate in patients with stable angina pectoris and applicable stenosis.”
Westra et al. found most of the mismatches between FFR and QFR at the 0.80 cutoff fell closely on either side of that threshold, where the benefit of treatment would likely approach the PCI-related event rate. However, they said randomized trials are needed to evaluate whether QFR calculation leads to noninferior clinical outcomes versus FFR in patients with intermediate stenosis.