Patients are responsible for a growing portion of healthcare costs. In some cases, that responsibility has become untenable, leading patients to delay or avoid care, or to leave their providers with unpaid bills. In their search for solutions, hospitals and practices are trying a variety of interventions.
Call it cost sharing or cost shifting, or explain it as exposing patients to the true cost of care. Regardless of how it’s framed, the outcome is that patients and their families have become responsible for a larger portion of medical costs. At the same time, prescription drug prices are continuing to rise, sometimes astronomically. As a result, some patients don’t seek the care they need when they need it. Others do obtain the medical care but, unable to pay the bills, leave physicians, practices and health systems with increasing levels of uncompensated care.
Each family has its own story, but across the population two primary drivers emerge: the increasing cost of prescription medications and the growing number of underinsured.
Swamped by rising drug costs
Spending on medications is projected to outpace growth in other parts of the healthcare sector this year, according to the Pew Charitable Trusts.
“Some of the new drugs—such as the injectable cholesterol drugs—are crazy expensive,” says Vincent Bufalino, MD, president of Advocate Medical Group in Chicago. “You know we’re talking 10, 12 grand a year for one drug.” He says the drugs are “phenomenal” but that few patients can afford them.
Net U.S. spending on pharmaceuticals is expected to reach between $370 and $400 billion by 2020, according to the American Heart Association (Circulation 2017;136[24]:e441-7). The authors make two key observations: (1) at least by some measurements, the market entry prices of many brand drugs and biologics are simply unaffordable for many patients; and (2) prices for established generic drugs have seen “sharp, rapid increases.” The authors point to digoxin and captopril which, between 2013 and 2014, increased 894 percent and 129 percent, respectively.
Even for patients who don’t require expensive medications, the cost of obtaining the care they need when they need it can be prohibitively high, especially for those with inadequate insurance coverage—the “underinsured.”
Insurance isn’t enough
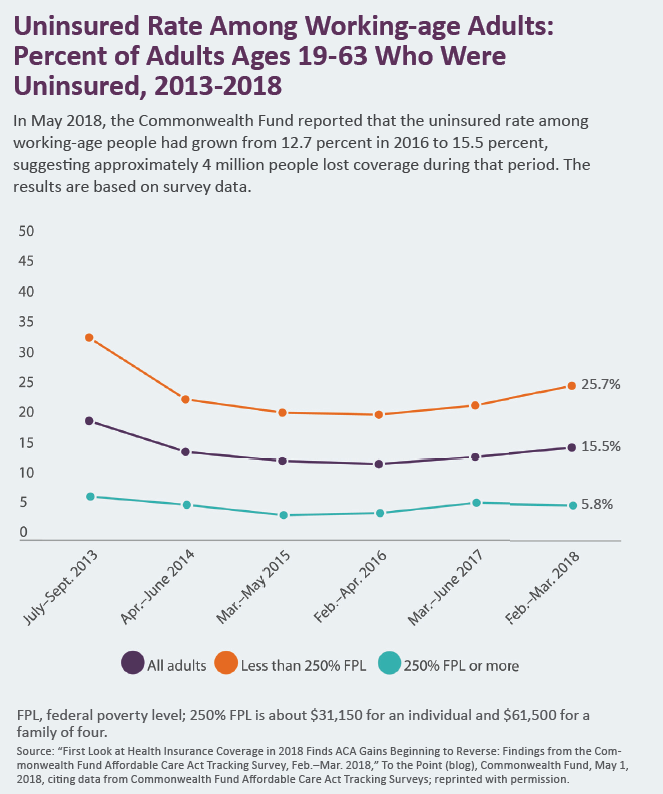
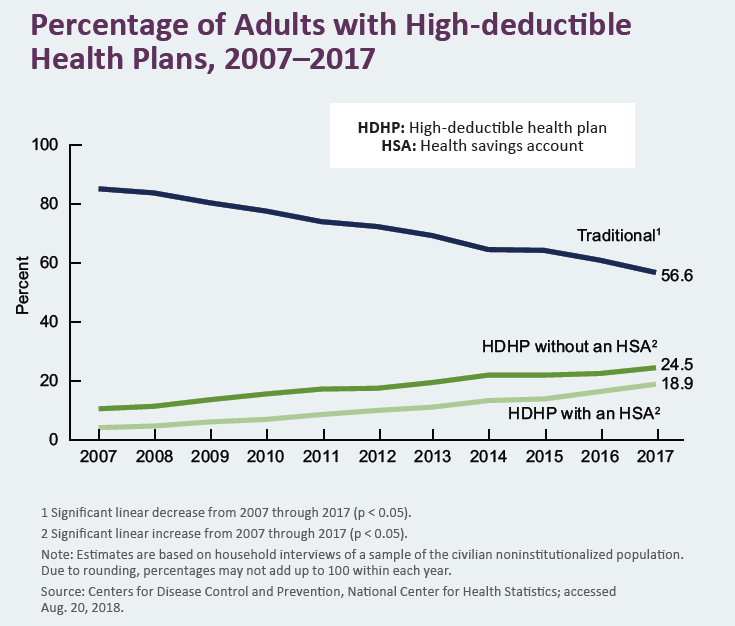
With less covered by insurance, patients are forced to shoulder more of the financial burden for their healthcare costs. A TransUnion Healthcare analysis revealed an 11 percent increase in average out-of-pocket costs between the fourth quarters of 2016 and 2017, while a Commonwealth Fund study found that those whose health coverage had deductibles of $3,000 or more grew from only 1 percent in 2003 to 13 percent in 2016.
“I think the most shocking development that we've seen is that many of our patients’ deductibles were around $5,000 to $10,000 a few years ago, but now we are seeing some plans with deductibles as high as $20,000,” says Todd M. Bankhead, vice president of clinical operation and surgical services at Wake Forest Baptist Health in Winston-Salem, N.C.
The Commonwealth Fund reported that 28 percent of working-age adults in the U.S. who had health insurance all year were underinsured in 2016, up from 23 percent in 2014. Of those considered underinsured (defined by the Commonwealth Fund as having high out-of-pocket expenses relative to their income), 45 percent went without needed healthcare because of cost.
Everyone suffers
The impact on patients is profound. The connection between increased cost of medications and poorer health outcomes has been well documented (Circulation 2017;136[24]:e441-7; PT 2012;37[1]:45-55).
Some patients also forgo care, as demonstrated by many examples in the literature. For example—
- Lack of health insurance and financial worries among those with health insurance have been associated with delays in seeking emergency care for myocardial infarction (JAMA 2010;303[14]:1392-1400).
- Between 2008 and 2016, increased use of prasugrel and ticagrelor (compared with clopidogrel) correlated with more prescriptions for P2Y12 inhibitors going unfilled. Adherence was worse in poorer areas (JAMA Intern Med 2018;178[7]:943-50).
Meanwhile, when patients can’t pay for services already rendered, their providers lose money. “Many organizations are lucky to collect 8 percent of accounts receivables for patient obligations, as medical bills are the number one reason for personal bankruptcy,” Bankhead says.
So, what to do? Physicians and health systems frequently provide uncompensated services and work to connect patients with outside resources. Payment plans and no-interest loans—always part of the picture—are becoming more common.
Shorten hospital stays
John A. Spertus, MD, MPH, clinical director of cardiovascular education and outcomes research at Saint Luke’s Mid America Heart Institute in Kansas City, Mo., thinks greater use of proactive risk stratification would go a long way toward reducing the time patients spend in the hospital, which would in turn lower costs for both patients and providers. As an example, he cites research on same-day discharge after elective percutaneous coronary intervention (PCI) at Barnes-Jewish Hospital in St. Louis.
By assessing—and then mitigating—patient risks, physicians were able to send most elective PCI patients home the same day, achieve high patient satisfaction and save the hospital an estimated $1.8 million annually (J Am Heart Assoc 2018;7[4]:e005733). “If they respond well to Lasix, and you can get a next-day follow up, why admit them to the hospital, where they incur more cost?” Spertus asks.
Not all solutions are clinical, however.
 Adopt a clinically integrated revenue cycle
Adopt a clinically integrated revenue cycle
Drawing on experience working in both academic and private healthcare settings, Bankhead calls for integrating revenue cycle processes into clinical workflow. He says embedding specially trained coders and revenue-integrity liaisons “elbow-to-elbow with clinical and operation staff ” helps ensure clinicians are knowledgeable about payer policies and common reasons for denial while supporting appropriate documentation. As a result, clinicians are better prepared for peer-to-peer conversations with payers’ medical directors, where the goal often is to overturn a denial.
Bankhead also recommends policy and process changes related to how patient payments are handled—especially for elective procedures.
- Full payment: Require payment in full prior to providing any elective procedures. That doesn’t mean turning away patients, Bankhead insists, but rather enlisting financial counselors and social workers to work with patients checking eligibility for public programs and charities, and, if all else fails, arranging no-interest loans.
- Backfill: When patients’ elective procedures end up being delayed, have a process to fast-track fully funded patients to optimize resources.
- Authorization/pre-certification: Insured patients must be approved. It seems obvious but, too often, patients end up being responsible for the full cost of their care because this step was neglected.
- No patient risk: None of these policies can create additional risk or exposure for the patient. “Obviously, ‘no margin, no mission,’” Bankhead says, “but ultimately we need to be much more proactive in taking into consideration our patients’ financial constraints and limitations.”
Wayne Hartley, AMGA’s chief operations officer, also emphasizes the importance of identifying financial concerns up front, allowing more time to find resources. He encourages practices to stay on top of hospital and health system guidelines and resources, and to know which pharmaceutical and device programs are available.
Adapt care plans, engage patients
If tackling financial issues begins in the exam room, physicians will have to factor in costs while talking with patients about care plans. One example, says Bufalino, is cutting back on the annual stress test for patients who have had coronary artery bypass graft surgery.
He also sees the focus moving upstream. “I would say I spend that much more time educating folks about diet, about exercise, about weight loss, about things they can do in their day-to-day lives that don't require drugs,” he explains. But he also talks about money.
Most physicians understand the need to educate patients about costs. But who has the resources to do it thoroughly? Results from a 2018 University of Utah Health survey found 64 percent of surveyed healthcare executives and clinicians think there isn’t enough time to discuss costs with patients, and 78 percent believe the tools they need for such discussions aren’t available. Physicians are nevertheless trying: Only 18 percent of the survey respondents said it’s not the physician’s responsibility to educate patients about costs (NEJM Catalyst, online July 10, 2018).
Patients need guidance, Bankhead stresses. He points out that many don’t understand their deductible thresholds, nor do they have a full appreciation for the total cost of care.
As physicians have clinical conversations with their patients, they need to take financial issues into consideration, Bufalino says. “It is really about your relationship with the patients.”
